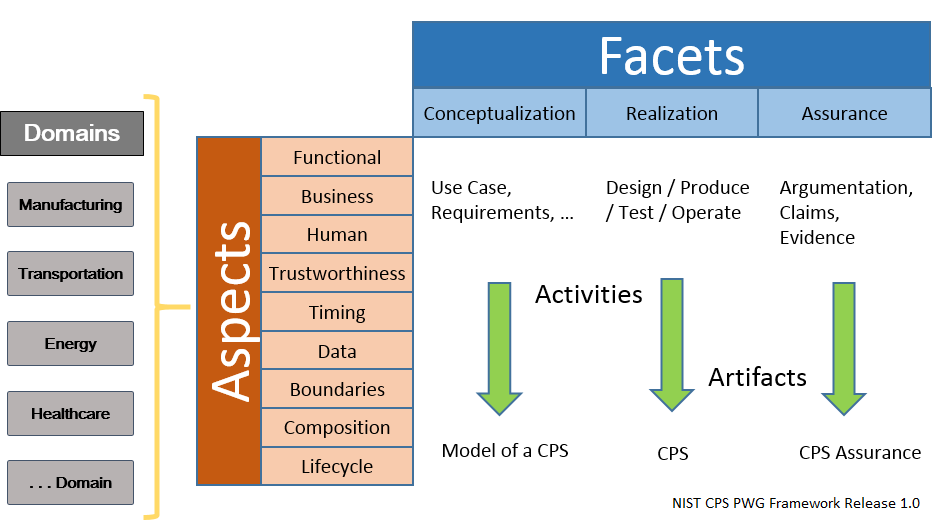
Facets Claim Processing System
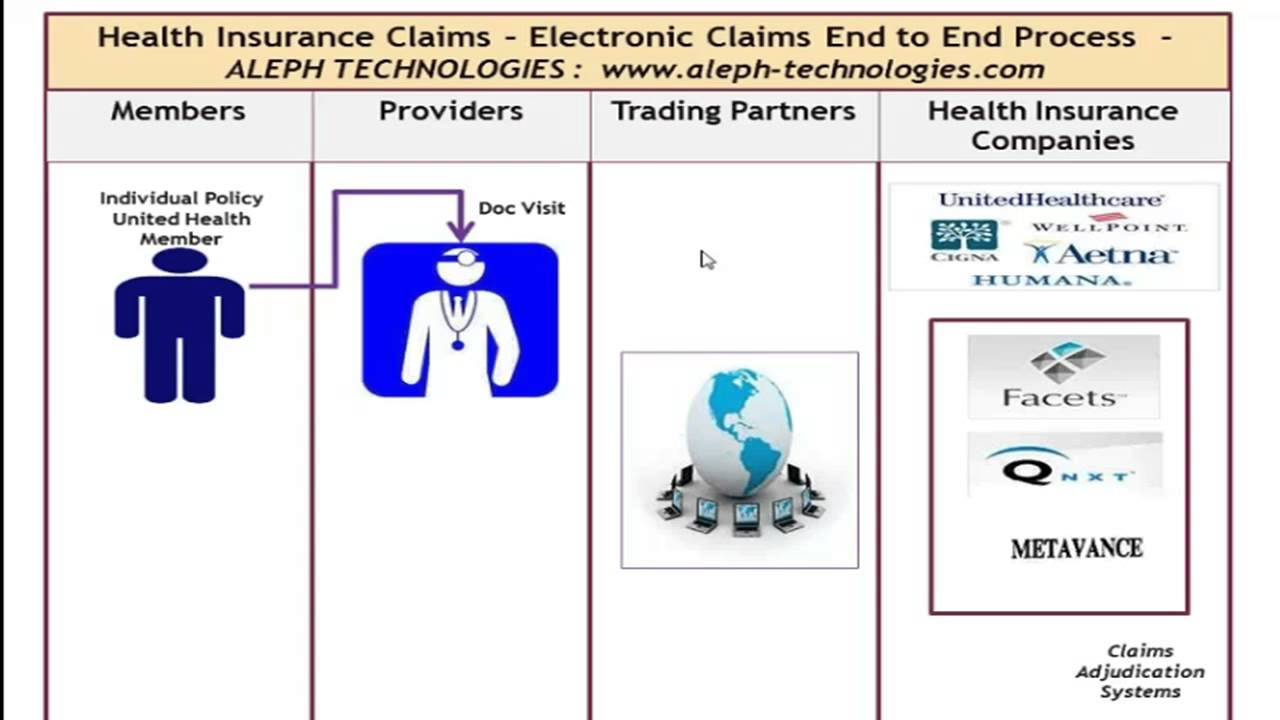
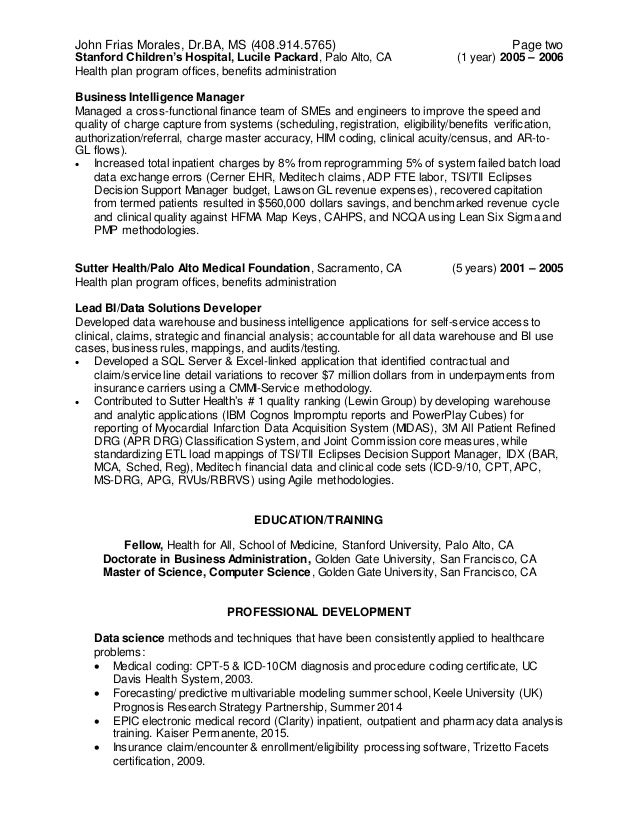
Facets claim processing system. The two most common claim forms are the CMS -1500 and the UB -04. A specific facility provider of service may also utilize this type of form. Claim Processing System case study Project Mission and Background.
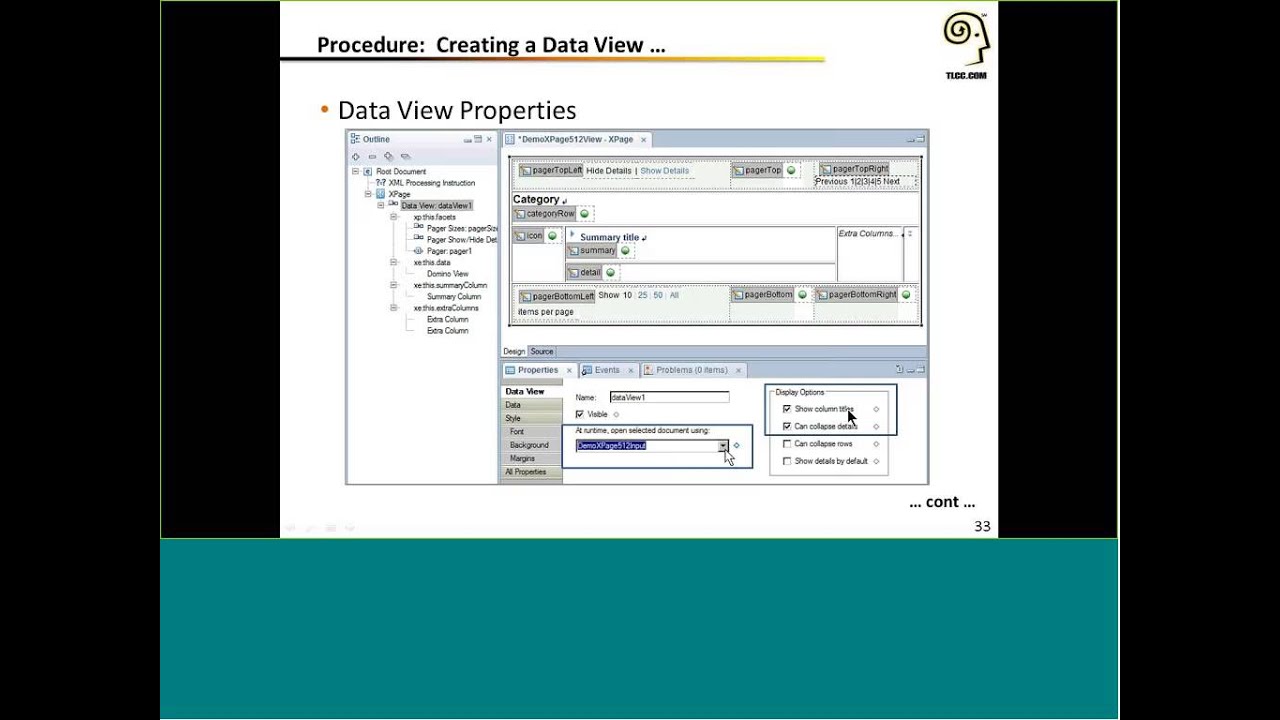
For more information on FACETS Claim processing please visit. What is trizetto facets. It helps the organizations to perform their day to day operational work by utilizing any or all of the application groups.
Winwinclick Faucet sites have been serving for a long time and processing satisfaction. A modular system which integrates consumer care and claims revenue management to help organizations which meets organizational needs and requirements that helps them to reach their goals. Facets is the industry-leading core administrative processing system today.
The websites you see above in the Navigation Menu have been set up in the same way and are functioning successfully. So what are the steps. It is currently processing millions of transactions per week for more than 80 health plans.
The Facets system automates and streamlines critical business functions across the enterprise including member enrollment premium billing claims processing and customer service helping payers decrease administrative spending while improving both healthcare and business. After the successful completion of Facets training the learners will be able to. Business Analysis in Healthcare Domain with Facets Training.
It is easy to search for data which you want it is a simple way that works through a module to join multiple which makes a fact. Who knows maybe you can become rich successfully. We configure agreements and pricing and validate the pricing using custom reports and Claim Processing.
To integrate with a plethora of existing systems while crossing through virtually Filename. The health plan had selected the TriZetto-hosted Facets product as the core claims processing system.
1-number of Facets specified in Facets F11.
We configure agreements and pricing and validate the pricing using custom reports and Claim Processing. Who knows maybe you can become rich successfully. It is used to process medical and hospital transactions or facility claims. The Facets system automates and streamlines critical business functions across the enterprise including member enrollment premium billing claims processing and customer service helping payers decrease administrative spending while improving both healthcare and business outcomes. Judges Facet 2. We configure agreements and pricing and validate the pricing using custom reports and Claim Processing. It is easy to search for data which you want it is a simple way that works through a module to join multiple which makes a fact. Facet number out of range. Lu0026F_Implementation_of_Facetspdf - Read File Online - Report Abuse.
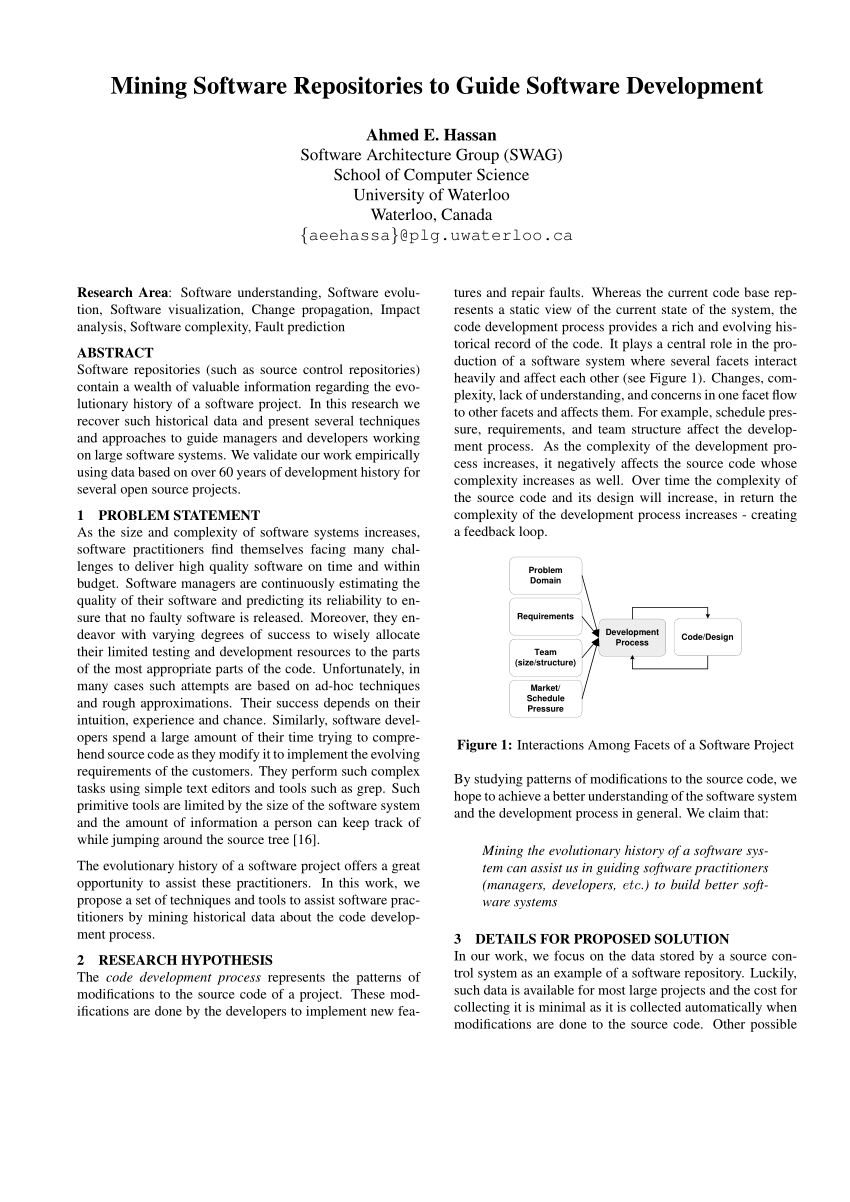
The Facets system automates and streamlines critical business functions across the enterprise including member enrollment premium billing claims processing and customer service helping payers decrease administrative spending while improving both healthcare and business outcomes. Facet number out of range. The two most common claim forms are the CMS -1500 and the UB -04. Specify your one Facets statement before other facet-related commands such as Positive2 to prevent incorrect standard values being used. Analyzed HIPAA 4010 and HIPAA 5010 standards for 837IP 27xs 834 and 835 transactions and prepared gap analysis document for each transaction. Facets is an integrated health care payer administration solution. Sometimes your company will give you user name and.


























Posting Komentar untuk "Facets Claim Processing System"